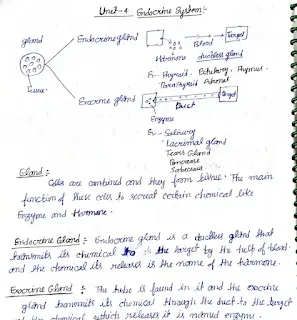
Autonomic and Endocrine Systems (HAP 2) - Handwritten Notes
Download handwritten notes for Human Anatomy and Physiology 2 (Semester 2), focusing on the Autonomic Nervous System (ANS) and its interaction with the Endocrine System. These notes cover the regulation of the ANS by the central nervous system, autonomic reflexes, the neuroeffector junction, and a detailed comparison of the sympathetic and parasympathetic divisions. They explain neurotransmitters (acetylcholine and norepinephrine), their receptors (cholinergic and adrenergic), and their removal mechanisms. The overall and specific functions of both sympathetic and parasympathetic systems, including the effects of catecholamines. Available as a PDF download.
Keywords: Autonomic Nervous System, ANS, Endocrine System, Sympathetic, Parasympathetic, Acetylcholine, Norepinephrine, Cholinergic Receptors, Adrenergic Receptors, Neuroeffector Junction, Catecholamines, Homeostasis, Autonomic Reflexes, Human Anatomy and Physiology, Handwritten Notes, PDF, Download, Semester 2, B.Pharm, CNS Regulation.
Autonomic and Endocrine Systems - Detailed Explanation
Introduction to the Autonomic Nervous System (ANS)
The autonomic nervous system (ANS) is a division of the peripheral nervous system that controls involuntary functions, such as heart rate, digestion, respiration, and glandular secretions. It plays a crucial role in maintaining homeostasis, the body's internal balance. The ANS works closely with the endocrine system, which uses hormones to regulate bodily functions. While the ANS provides rapid, short-term control, the endocrine system provides slower, longer-lasting control.
Central Nervous System Regulation of the ANS
Various regions of the central nervous system (CNS), particularly the hypothalamus, brainstem, and spinal cord, regulate autonomic nervous system function. The hypothalamus is a key integration center, receiving sensory input and coordinating appropriate autonomic responses. The brainstem contains centers that control vital functions like breathing and heart rate. The spinal cord contains reflex centers for activities like urination and defecation.
Autonomic Reflexes and Homeostasis
Autonomic reflexes contribute to homeostasis by automatically adjusting physiological processes in response to changes in the internal environment. These reflexes involve sensory receptors, afferent (sensory) neurons, integration centers in the CNS, efferent (motor) neurons, and effector organs (e.g., smooth muscle, cardiac muscle, glands). Examples include the baroreceptor reflex (regulating blood pressure) and the pupillary light reflex.
The Neuroeffector Junction
The neuroeffector junction in the ANS differs from a neuron-to-neuron synapse. In the ANS, the postganglionic neuron releases neurotransmitters from varicosities (swellings) along its axon, rather than a single axon terminal. This allows for a more diffuse release of neurotransmitters, affecting a larger area of the effector tissue. The receptors on the effector cells are also distributed more widely.
Comparison of Sympathetic and Parasympathetic Systems
The ANS has two main divisions: the sympathetic and parasympathetic systems. They often have opposing effects on target organs, providing a fine-tuned control mechanism.
Anatomical Features:
- Sympathetic: Preganglionic neurons originate in the thoracolumbar region of the spinal cord (T1-L2). Ganglia are located near the spinal cord (sympathetic trunk ganglia and prevertebral ganglia). Preganglionic fibers are short, and postganglionic fibers are long.
- Parasympathetic: Preganglionic neurons originate in the brainstem (cranial nerves III, VII, IX, X) and the sacral region of the spinal cord (S2-S4). Ganglia are located near or within the effector organs (terminal ganglia). Preganglionic fibers are long, and postganglionic fibers are short.
Autonomic Neurotransmitters and Receptors
Neurotransmitters:
- Acetylcholine (ACh): Released by all preganglionic neurons (both sympathetic and parasympathetic) and all parasympathetic postganglionic neurons. Also released by *some* sympathetic postganglionic neurons (e.g., those innervating sweat glands).
- Norepinephrine (NE): Released by most sympathetic postganglionic neurons.
Receptors:
- Cholinergic Receptors (bind ACh):
- Nicotinic receptors: Found on all postganglionic neurons (both sympathetic and parasympathetic) and at the neuromuscular junction of skeletal muscle. Always excitatory.
- Muscarinic receptors: Found on effector cells innervated by parasympathetic postganglionic neurons. Can be excitatory or inhibitory, depending on the subtype.
- Adrenergic Receptors (bind NE and epinephrine):
- Alpha receptors (α1, α2): Generally excitatory, except for α2 receptors in the gut, which are inhibitory.
- Beta receptors (β1, β2, β3): β1 receptors are generally excitatory (especially in the heart), β2 receptors are generally inhibitory (e.g., causing bronchodilation), and β3 receptors are involved in lipolysis.
Neurotransmitter Removal Mechanisms
Neurotransmitters are removed from the synaptic cleft (or neuroeffector junction) to terminate their action. This can occur through:
- Reuptake: The neurotransmitter is taken back up into the presynaptic neuron (e.g., norepinephrine).
- Enzymatic degradation: The neurotransmitter is broken down by enzymes (e.g., acetylcholinesterase breaks down acetylcholine).
- Diffusion: The neurotransmitter diffuses away from the synapse.
Functions of the Sympathetic System
The sympathetic system is often called the "fight-or-flight" system. It prepares the body for stressful or emergency situations. Overall functions include:
- Increased heart rate and contractility.
- Increased blood pressure.
- Bronchodilation (widening of airways).
- Increased blood glucose levels.
- Dilation of pupils.
- Redirection of blood flow from the skin and digestive organs to skeletal muscles.
- Decreased digestive activity.
Specific functions: Include stimulation of sweat glands, constriction of blood vessels in the skin, and release of epinephrine and norepinephrine from the adrenal medulla.
Functions of the Parasympathetic System
The parasympathetic system is often called the "rest-and-digest" system. It promotes energy conservation and maintenance functions. Overall functions include:
- Decreased heart rate.
- Increased digestive activity (increased salivation, gastric motility, and secretion).
- Constriction of pupils.
- Bronchoconstriction (narrowing of airways).
- Increased activity of glands involved in digestion.
Specific Functions: Include control of bladder emptying, defecation, and lacrimation (tear production).
Catecholamines vs. Direct Sympathetic Stimulation
The effects of catecholamines (epinephrine and norepinephrine released from the adrenal medulla) are similar to those of direct sympathetic stimulation, but they are more prolonged because the hormones circulate in the bloodstream. Catecholamines can also reach tissues not directly innervated by sympathetic fibers.
Parasympathetic Division - Detailed Anatomy (From Provided Text)
Preganglionic neurons of the parasympathetic system arise from several nuclei of the brainstem and from the sacral region of the spinal cord (segments S2 to S4). The axons of the preganglionic neurons are quite long compared to those of the sympathetic system and synapse with postganglionic neurons within terminal ganglia that are close to or embedded within the effector tissues. The very short axons of the postganglionic neurons then provide input to the cells of that effector tissue.
The preganglionic neurons that arise from the brainstem exit the CNS through cranial nerves. The oculomotor nerve (III) innervates the eyes; the facial nerve (VII) innervates the lacrimal gland, salivary glands, and mucus membranes of the nasal cavity; the glossopharyngeal nerve (IX) innervates the parotid (salivary) gland; and the vagus nerve (X) innervates the viscera of the thorax and abdomen (e.g., heart, lungs, stomach, intestines, and pancreas). The physiological significance of this latter nerve in terms of influence of the parasympathetic system is clearly illustrated by its widespread distribution and the fact that 75% of all parasympathetic fibers are in the vagus nerve. Preganglionic neurons that arise from the sacral region of the spinal cord exit the CNS and join together to form the pelvic nerves. These nerves innervate the viscera of the pelvic cavity (e.g., urinary bladder, colon).
Because the terminal ganglia are located within the innervated tissue, there is typically little divergence in the parasympathetic system compared to the sympathetic system. In many organs, the ratio of preganglionic fibers to postganglionic fibers is 1:1. Therefore, the effects of the parasympathetic system tend to be more discrete and localized, with only specific tissues stimulated at any given moment, compared to the sympathetic system in which a more diffuse discharge is possible.
Neurotransmitters of the Autonomic Nervous System (From Provided Text - Summarized)
The two most common neurotransmitters released by neurons of the ANS are acetylcholine (ACh) and norepinephrine (NE). Nerve fibers that release acetylcholine are referred to as cholinergic fibers and include all preganglionic fibers of the ANS — sympathetic and parasympathetic systems; all postganglionic fibers of the parasympathetic system; and sympathetic postganglionic (covered above).
Conclusion
The autonomic nervous system and the endocrine system work together, often in a coordinated manner, to maintain the body's internal environment. Understanding the intricate details of their anatomy, neurotransmitters, receptors, and functions is crucial for comprehending how the body regulates its many physiological processes.
Info!
If you are the copyright owner of this document and want to report it, please visit the copyright infringement notice page to submit a report.