Cephalosporin PDF Notes: Downloadable Resource
Download comprehensive notes on cephalosporin antibiotics in PDF format. These notes cover the different generations of cephalosporins (1st, 2nd, 3rd, 4th, and 5th), their antibacterial spectrum, mechanisms of action, clinical uses, pharmacokinetic properties, and potential side effects. Ideal for students, researchers, and healthcare professionals. Download now for convenient offline access.
Keywords: Cephalosporins, PDF, Download, Notes, Antibiotics, Beta-Lactams, Antibacterial, First Generation, Second Generation, Third Generation, Fourth Generation, Fifth Generation, Mechanism of Action, Side Effects, Pharmacology, Pharmacokinetics, Clinical Uses, Bacterial Resistance, Gram-Positive, Gram-Negative.
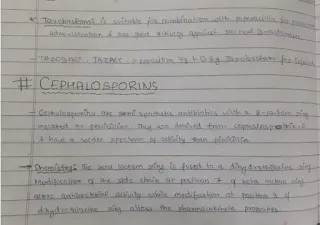
Cephalosporins: Generations, Mechanisms, and Uses
Cephalosporins are a large and important class of beta-lactam antibiotics. Like penicillins, they inhibit bacterial cell wall synthesis by binding to and inactivating penicillin-binding proteins (PBPs), leading to bacterial cell lysis and death. Cephalosporins are generally more resistant to beta-lactamases than many penicillins, making them effective against a broader range of bacteria. This document provides a detailed overview of cephalosporins.
Mechanism of Action
Cephalosporins, as beta-lactam antibiotics, share the same core mechanism:
- Inhibition of Transpeptidases (PBPs): Cephalosporins bind to and inhibit penicillin-binding proteins (PBPs), also known as transpeptidases. These enzymes are essential for the final step of peptidoglycan synthesis – the cross-linking of peptide chains in the bacterial cell wall.
- Weakening of Cell Wall: By inhibiting PBPs, cephalosporins prevent the formation of these crucial cross-links, weakening the cell wall.
- Bacterial Cell Lysis: The weakened cell wall is unable to withstand the osmotic pressure inside the bacterial cell, leading to cell lysis (bursting) and bacterial death. Cephalosporins are bactericidal.
Classification of Cephalosporins (Generations)
Cephalosporins are classified into five generations based on their antibacterial spectrum and resistance to beta-lactamases. As you move from the first to the fifth generation, the activity against Gram-negative bacteria generally increases, while the activity against Gram-positive bacteria may decrease (although some later-generation cephalosporins retain good Gram-positive activity).
- First-Generation Cephalosporins:
- Examples: Cefazolin (IV/IM), Cephalexin (oral), Cefadroxil (oral)
- Spectrum: Good activity against Gram-positive cocci (e.g., *Staphylococcus aureus* (but not MRSA), *Streptococcus pyogenes*). Limited activity against Gram-negative bacteria.
- Uses: Skin and soft tissue infections, surgical prophylaxis, urinary tract infections (caused by susceptible organisms).
- Second-Generation Cephalosporins:
- Examples: Cefuroxime (IV/IM/oral), Cefaclor (oral), Cefoxitin (IV/IM), Cefotetan (IV/IM)
- Spectrum: Increased activity against Gram-negative bacteria compared to first-generation cephalosporins (e.g., *Haemophilus influenzae*, some *Enterobacteriaceae*). Some have activity against anaerobes (cefoxitin, cefotetan). Retain good activity against Gram-positive cocci.
- Uses: Respiratory tract infections, intra-abdominal infections (cefoxitin, cefotetan), skin and soft tissue infections, urinary tract infections.
- Third-Generation Cephalosporins:
- Examples: Ceftriaxone (IV/IM), Cefotaxime (IV/IM), Ceftazidime (IV/IM), Cefdinir (oral), Cefpodoxime (oral), Ceftibuten (oral)
- Spectrum: Further increased activity against Gram-negative bacteria, including some *Pseudomonas aeruginosa* (ceftazidime). Less activity against Gram-positive cocci compared to first and second-generation cephalosporins. Some can cross the blood-brain barrier (ceftriaxone, cefotaxime).
- Uses: Serious Gram-negative infections, meningitis (ceftriaxone, cefotaxime), hospital-acquired pneumonia, gonorrhea (ceftriaxone), Lyme disease (ceftriaxone).
- Fourth-Generation Cephalosporins:
- Examples: Cefepime (IV/IM)
- Spectrum: Broad spectrum of activity, including good activity against both Gram-positive and Gram-negative bacteria, including *Pseudomonas aeruginosa*. More resistant to some beta-lactamases than third-generation cephalosporins.
- Uses: Hospital-acquired pneumonia, febrile neutropenia, complicated intra-abdominal infections, complicated urinary tract infections.
- Fifth-Generation Cephalosporins:
- Examples: Ceftaroline (IV)
- Spectrum: Active against methicillin-resistant *Staphylococcus aureus* (MRSA) and other resistant Gram-positive bacteria. Also has activity against some Gram-negative bacteria.
- Uses: Complicated skin and soft tissue infections, community-acquired pneumonia.
- Investigational:
- Examples: Ceftobiprole.
Pharmacokinetics
The pharmacokinetic properties of cephalosporins vary depending on the specific drug. Some key points:
- Administration: Cephalosporins can be administered orally, intravenously (IV), or intramuscularly (IM).
- Distribution: Most cephalosporins distribute well into body tissues and fluids. Some (e.g., ceftriaxone, cefotaxime) penetrate the cerebrospinal fluid (CSF) well, making them useful for treating meningitis.
- Elimination: Most cephalosporins are primarily eliminated by the kidneys. Dosage adjustments are often necessary in patients with kidney impairment. Ceftriaxone is an exception, as it is also eliminated in the bile.
Side Effects
Cephalosporins are generally well-tolerated, but they can cause side effects:
- Hypersensitivity Reactions: Allergic reactions, ranging from mild skin rashes to life-threatening anaphylaxis, can occur. Patients with a history of penicillin allergy may also be allergic to cephalosporins (cross-reactivity), although the risk is relatively low, especially with later-generation cephalosporins.
- Gastrointestinal Disturbances: Nausea, vomiting, diarrhea.
- Hematologic Effects: Rarely, cephalosporins can cause hematologic abnormalities, such as leukopenia (low white blood cell count), thrombocytopenia (low platelet count), or hemolytic anemia.
- Nephrotoxicity: Rare, but can occur, especially with high doses or in patients with pre-existing kidney disease.
- Disulfiram-like Reaction: Some cephalosporins (e.g., cefotetan, cefoperazone) can cause a disulfiram-like reaction when taken with alcohol. This reaction is characterized by flushing, headache, nausea, vomiting, and chest pain.
- Superinfections: Like other broad-spectrum antibiotics, cephalosporins can disrupt the normal gut flora, leading to superinfections, such as *Clostridioides difficile* infection (CDI).
Bacterial Resistance
- Bacteria can develop resistance to cephalosporins through several mechanisms:
- Beta-Lactamase Production: The most common mechanism. Many bacteria produce beta-lactamases that can inactivate cephalosporins. Extended-spectrum beta-lactamases (ESBLs) can hydrolyze a wide range of beta-lactam antibiotics, including many cephalosporins.
- Altered PBPs: Mutations in the genes encoding PBPs can lead to the production of PBPs with reduced affinity for cephalosporins.
- Decreased Permeability: Changes in the outer membrane of Gram-negative bacteria can reduce the penetration of cephalosporins.
- Efflux Pumps: Some bacteria have efflux pumps that actively pump cephalosporins out of the cell.
Info!
If you are the copyright owner of this document and want to report it, please visit the copyright infringement notice page to submit a report.